You are here
Understanding Spasticity Following Spinal Cord Injury
Speakers
Abstract
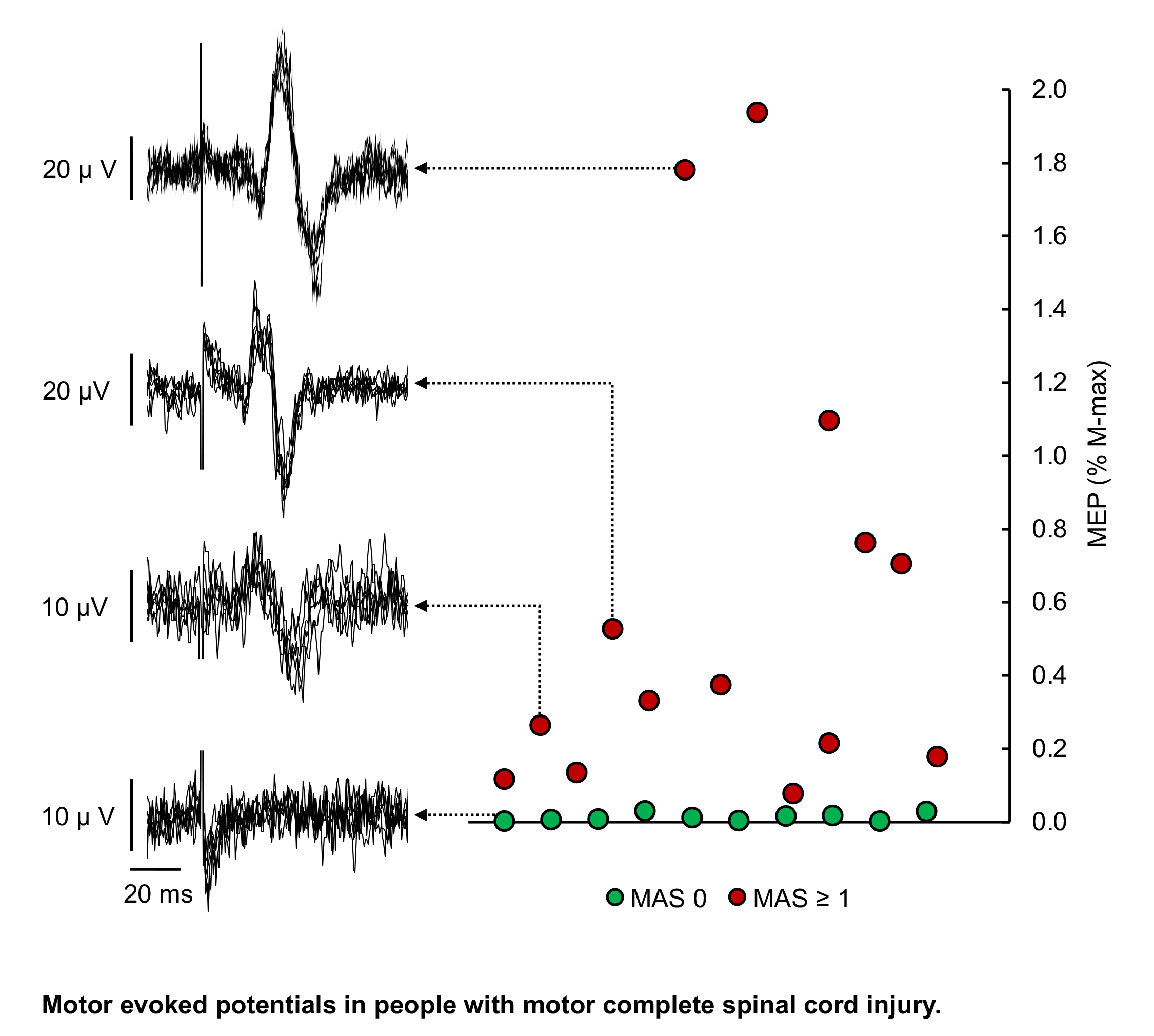
Spasticity is one of the most common symptoms manifested following spinal cord injury (SCI). The aim of the study was to assess spasticity in people with subacute and chronic SCI with different severity injury standardizing the time and assessments of spasticity. We tested 110 individuals with SCI classified by the American Spinal Injury Association Impairment Scale (AIS) as motor complete (AIS A and B; subacute, n=25; chronic, n=33) or motor incomplete (AIS C and D; subacute, n=23; chronic, n=29) at a similar time post-injury (subacute=~1-month post-injury during inpatient rehabilitation and chronic=>1-year post-injury) using a clinical (Modified Ashworth Scale) and kinematic (Pendulum test) outcomes to assess spasticity in the quadriceps femoris muscle. Using both methodologies, we found that among participants with subacute motor complete injuries, a small percentage of them showed spasticity while the majority showed no spasticity. In contrast, among people with subacute motor incomplete injury, both methodologies revealed that most individuals showed spasticity while only a small percentage showed no spasticity. In chronic injuries, most participants showed spasticity regardless of injury severity. Notably, when spasticity was present, its magnitude was similar across injury severity in subacute and chronic injuries. Our results suggest that the prevalence, but not the magnitude, of spasticity differs between individuals with motor complete and incomplete SCI in the subacute and chronic stage of the injury. We argue that considering the 'presence of spasticity' might help the stratification of participants with motor complete injuries for clinical trials.