You are here
Prediction of Response to Intensive Treatment with Arm Practice in Chronic Stroke
Speakers
Abstract
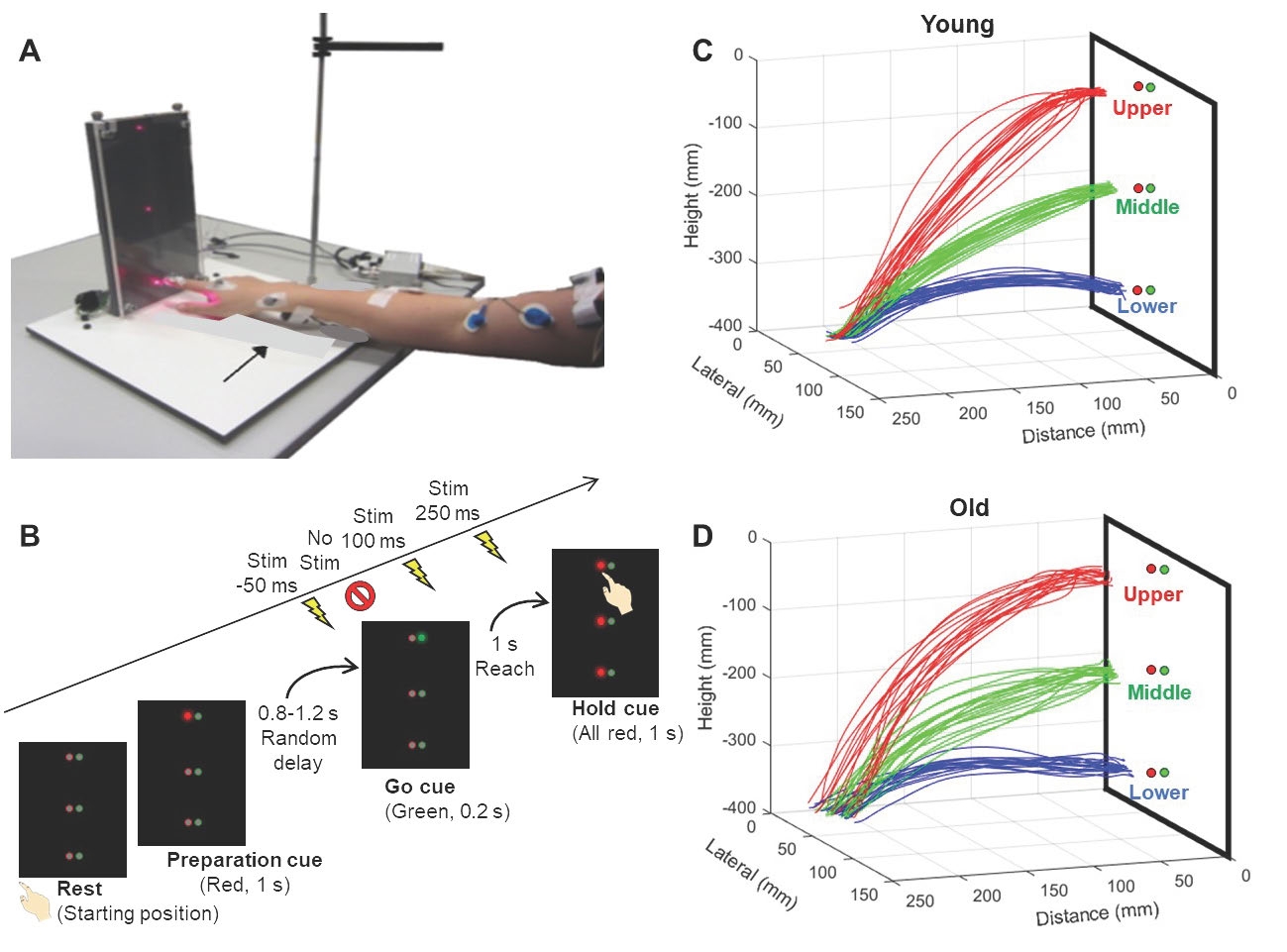
Introduction: Upper extremity motor impairment is common and persistent after stroke. Methods based on guided, repetitive, task practice such as Constraint-induced Therapy and robotic rehabilitation has been shown to be effective in reducing impairment in populations of chronic stroke patients, but individual responses are highly variable. If baseline measures could be used to predict response to an intervention, then it would be possible to establish realistic rehabilitation goals and effectively allocate resources. The predictive model might could also provide insight into the biological and psychological substrates for response to therapy. Our aims in this study were to address these goals of prediction and understanding of mechanism in patients with chronic hemiparesis after stroke. Methods. The intervention used a combination of robot-assisted therapy (75% session time) and functional arm use in real-world tasks related to the robotic movements practiced in the session (25% session time.) Participants had 12 intervention sessions over 12 weeks. Baseline measures include the Upper Extremity Fugl-Meyer Assessment, Wolf Motor Function Test, Action Research Arm Test, Stroke Impact Scale, questionnaires on pain and expectancy, MRI, transcranial magnetic stimulation multiple muscle mapping, kinematics, wearable-based accelerometry, and genomic testing. The goal of the prediction methods was to predict a clinically meaningful (≥ 5 point) increase in Fugl-Meyer using logistic regression. Results. The average increase in Fugl-Meyer was 4.6 ± 1.0 SE, and median increase 2.5. Approximately one-third of participants had a clinically meaningful response to the intervention. The selected logistic regression model had a receiver operating curve with AUC=0.99 (Std Error = 0.01, 95% Wald confidence limits: 0.967 - 1) that showed little evidence of overfitting. Six variables that predicted response represented impairment, functional, and genomic measures, including time after stroke, whether dominant side was affected, proprioceptive function, time to complete Wolf Motor Function tasks, grip strength, and Klotho genotype. TMS and MRI measures did not survive the variable selection process. Most outcomes derived from wearable data did not change significantly over the course of the intervention. Conclusion. A simple weighted sum of six baseline factors can accurately predict clinically meaningful impairment reduction after outpatient intensive practice intervention in chronic stroke. While goals for people affected by stroke include better ability to participate in desired activities, reduction of impairment may be a critical first step to those goals. Further validation and generalization of this model will increase its utility in clinical decision-making.