You are here
The Neurovascular Pathobiology of Alzheimer’s Disease
Speakers
Abstract
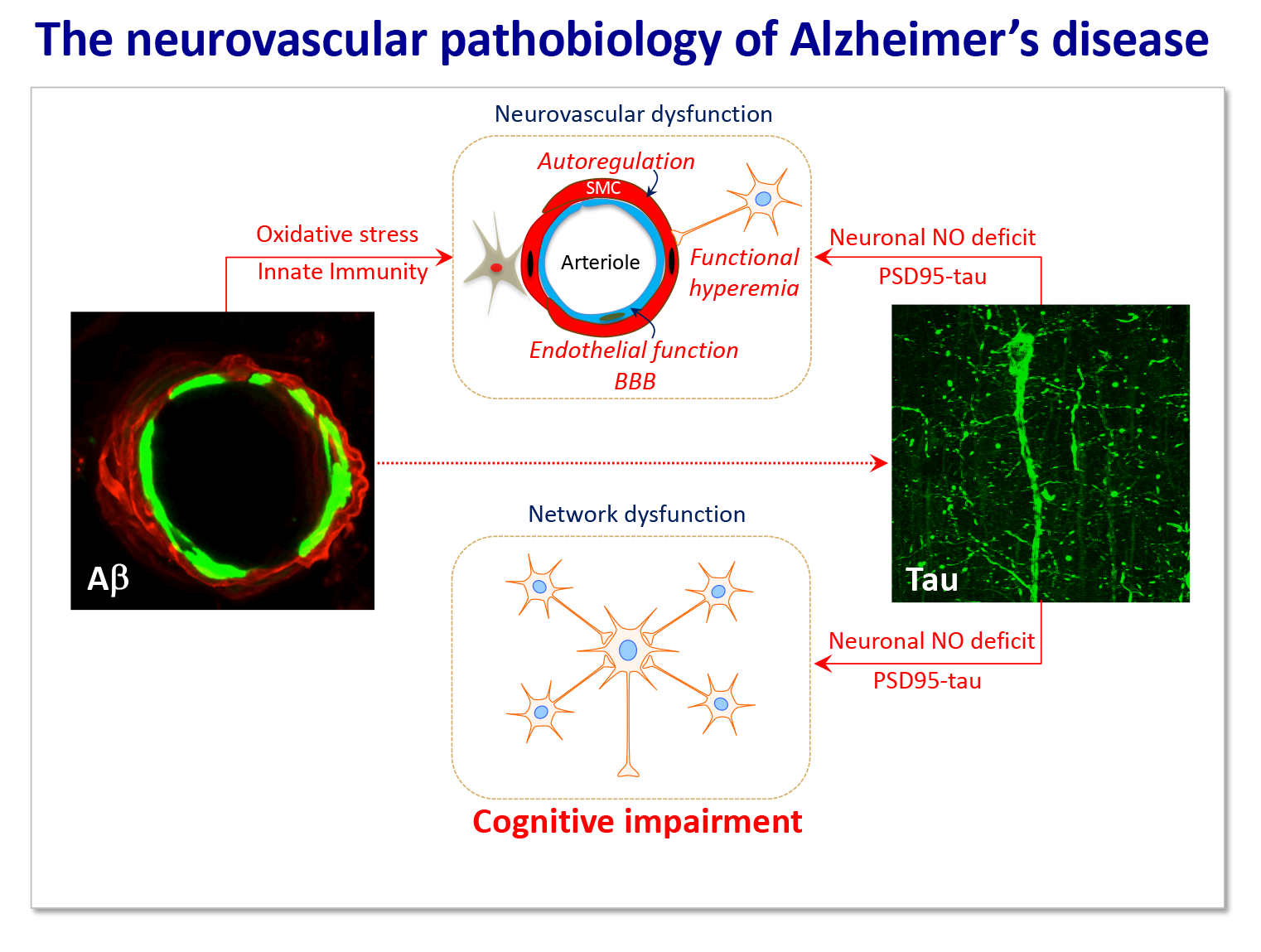
The brain is uniquely dependent on a well-regulated delivery of oxygen and glucose through the blood supply. If the delivery of cerebral blood flow is not adequate to maintain the energetic and metabolic homeostasis of working brain cells, brain dysfunction and damage ensues. Although the mechanisms of the cognitive dysfunction caused by vascular factors (vascular cognitive impairment) or neurodegeneration (Alzheimer’s disease, AD) have traditionally been considered distinct, there is increasing evidence that alterations in cerebral blood vessels play a role both in vascular and neurodegenerative dementias. Clinical-pathological and imaging studies support the notion that vascular dysfunction is an early manifestation of AD and aggravates the deleterious effects of AD pathology by reducing the threshold for cognitive impairment and accelerating the pace of the dementia. Indeed, amyloid-beta and tau, major pathogenic factors in AD, have profound cerebrovascular effects. Amyloid-beta impairs the structure and function of cerebral blood vessels and associated cells (neurovascular unit) by activating innate immune cells and leading to vascular oxidative stress and inflammation. Pathological tau suppresses glutamate-dependent production of nitric oxide, which, in turn, dampens the increase in blood flow produced by synaptic activity, but also leads to interneuron network dysfunction and increased excitability. These finding, collectively, indicate that vascular alterations are important factors in AD pathobiology. In the absence of mechanism-based approaches to counteract dementia, targeting cerebrovascular function may offer the opportunity to mitigate the public health impact of one of the most disabling human afflictions.