You are here
Investigating the Role of the Adaptive Immune System in Stroke-Induced Injury and Recovery
Speakers
Abstract
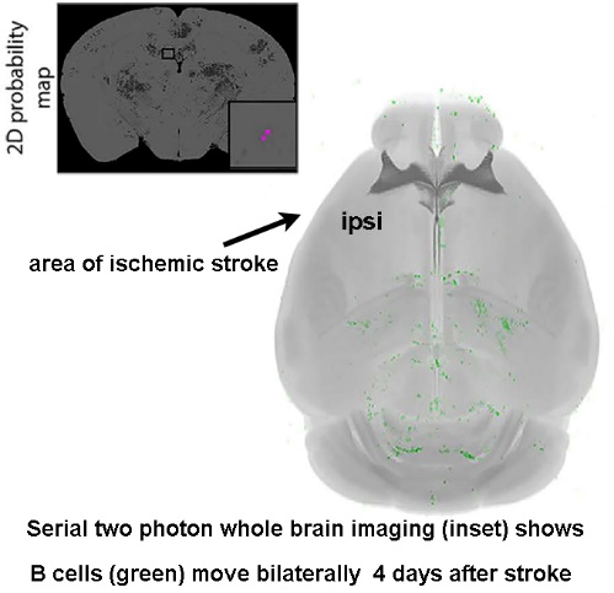
My overarching hypothesis is that the immune system – driven by an autoreactivity to CNS-derived antigens – plays a fundamental role in neuronal plasticity within the CNS. B cells, T cells, and natural killer (NK) T cells comprise the adaptive component of the immune system and can mediate long-term immune responses after stroke. To this end, my recent studies show that B cells diapedese bilaterally into the post-stroke brain (image), particularly into areas mediating cognitive recovery e.g. hippocampal dentate gyrus. Furthermore, long-term B cell depletion impedes motor and cognitive recovery after focal ischemic stroke in mice. Although I use preclinical studies to investigate the mechanisms by which adaptive immune responses affect post-stroke plasticity (e.g., protection from excitotoxicity, dendritic pruning), it is critical to concomitantly confirm and characterize these cells in humans. My clinical studies into the role of neuroinflammation during brain injury and repair has expanded beyond the field of ischemic stroke to also include subjects with amnestic mild cognitive impairment and pediatric patients on ventilator and hemodynamic support who experience stroke. The combination of preclinical and clinical studies reflects both my own training, which included a clinical postdoctoral fellowship, and my ongoing scientific philosophy that translational research will hasten the collective understanding of functional recovery during and following brain injury.