You are here
Creating and Validating a New Tool to Detect Delirium
Speakers
Abstract
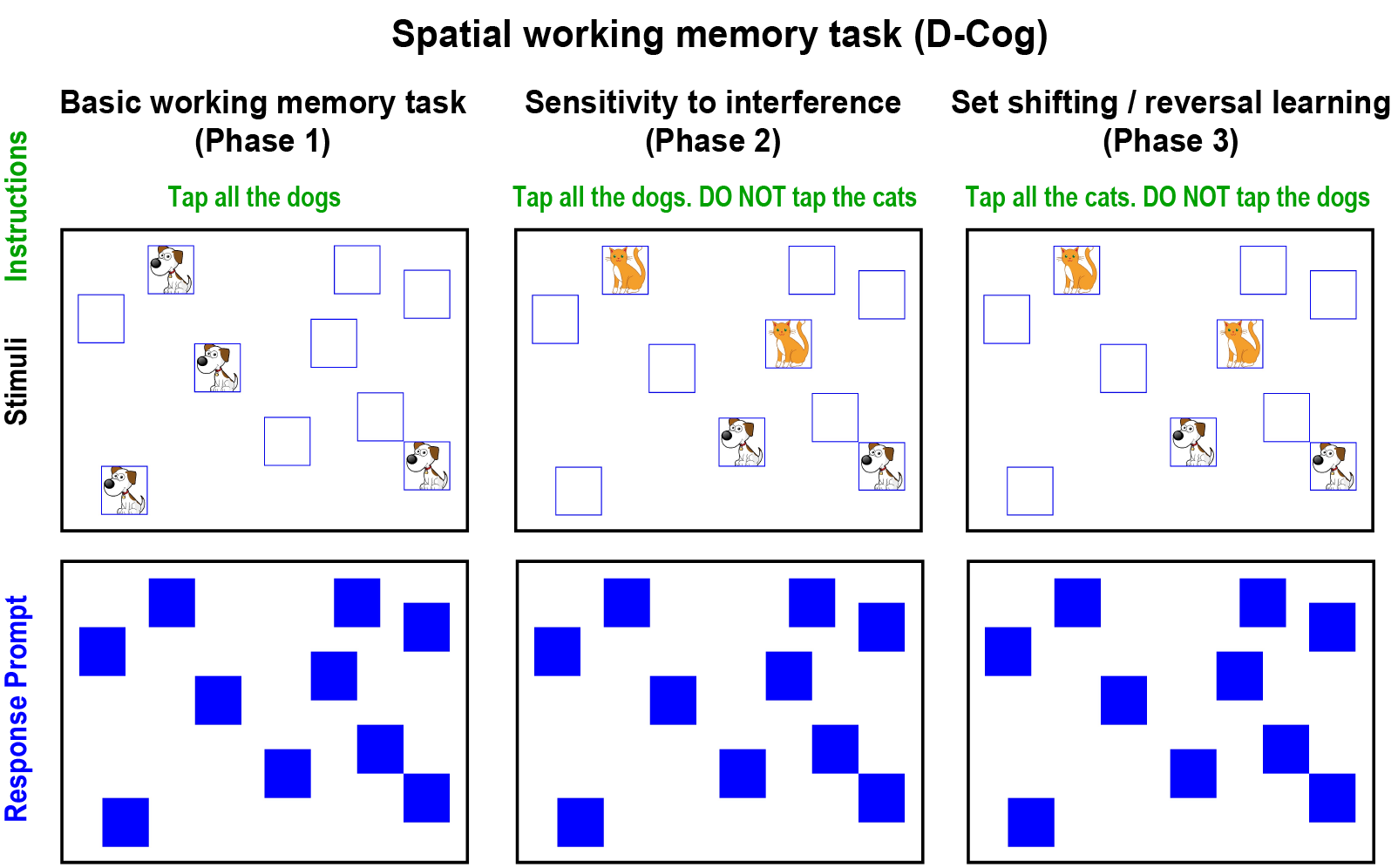
The most common neurological complication in hospitalized patients, delirium, has been repeatedly shown to be dramatically under-recognized, with as few as 1 in 8 cases diagnosed. A number of diagnostic tools exist but are underutilized due to requirements for specific/special training, time consuming administration, and complex scoring procedures. Moreover, the development of improved tools has been hampered by the lack of a definitive marker for delirium, so that the evaluation of new tools has relied on the opinions of expert consensus panels for measuring their classification accuracy. Here we introduce both a new tool for assessing delirium and a novel model system for testing diagnostic instruments. The tool generates a scale based on spatial working memory ability that can be digitally administered in a 1-2 minute time window and scored automatically using a handheld tablet. The model system was developed with participants receiving ECT treatments, both before seizure administration and after it, during the resulting period of postictal delirium. Comparing this new tool, the D-Cog, to 7 existing widely used cognitive tests sensitive to delirium, including months of the year backwards and digit span, we found that the D-Cog was comparable to (5 of 7) or better than (2 of 7) the standard tasks using a cutoff to maximize classification accuracy. When comparing baseline performance to post-ECT results (paired analysis), the D-Cog outperformed 6 of the 7 tests. Moreover, we found that classification errors were reduced by a factor of 5, from 24% to 4%, for the paired data from the D-Cog, and by a factor of 2, from 26% to 14%, for the paired data when considering all tests that we studied. These results suggest that changes in spatial working memory may be a highly accurate marker for delirium, and that the incorporation of baseline test data into clinical decision making may dramatically improve the assessment of delirium.